Concussion
Welcome to Dr Khurana’s Concussion pageSee the PDF at the bottom of this page for our review on Concussion including a brief overview of “Chronic Traumatic Encephalopathy” (CTE) which has recently been found to be present in almost 100% of brains of deceased US NFL players who donated their brains for medical scientific analysis. CTE is likely to be present in many Australian AFL and NRL players, and there are obvious implications for children with repeat sports concussions.
CONCUSSION
“Concussion” is defined as a sudden, transient alteration of consciousness induced by traumatic biomechanical forces transmitted directly or indirectly to the brain. Concussion does involve some period of transient amnesia (especially ‘antegrade’).
The term concussion:
- Is derived from the Latin word “concutere“, which means ‘to shake violently’;
- Should NOT be used interchangeably with “mild traumatic brain injury” or “post-concussion syndrome”;
- Should not be trivialised by using inappropriate terms such as “knock” and “ding” in a concussed sports player.
Forces that cause concussion are typically strong and “rotational” forces (higher G-force) that shear brain tissue directly or indirectly. Lower G- (and also perhaps more “linear” / less rotational) forces might not cause concussion and are referred to as sub-concussive forces. However, repeated sub-concussive forces may still damage brain structure and function in the longer term.
Concussion is very common. In Australia, in the AFL code alone there are 6 to 7 concussions per team per season, and in the U.S.A., the Centers for Disease Control (CDC) reports there are approximately 4 million sports concussions per year in that country alone.
The most common (reported) symptoms of concussion are “headache”, dizziness (this could be ‘off balance’, ‘light headed’, or ‘woozy’ etc.) and confusion.
The common (observed) signs of concussion are a dazed appearance, disorientation to (e.g.,) game details, and impairment of balance and coordination. In only 10% of sports concussion patients is there an actual loss of consciousness (but there is a transient alteration of consciousness in 100%, by definition).
Most sports concussion patients will not have identifiable pathology on routine investigations such as CT and regular MRI; some however will have, particularly in more severe instances.
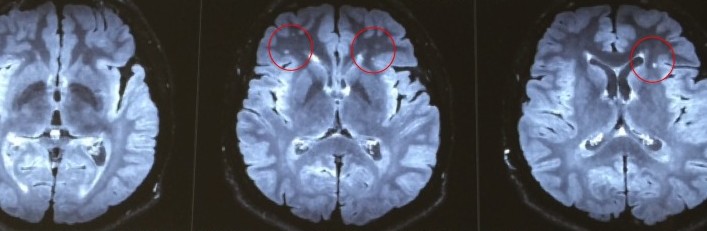
The MRI image below (FLAIR sequence) is from of a young concussed patient (a motor vehicle accident in this case) and shows punctate cerebral white matter changes (circled in red below) consistent with diffuse axonal injury (DAI) from rotational forces causing axonal shear.
Using more specialised MRI scanning modalities (e.g., MR tractography and functional MRI), structural abnormalities may be more readily detectable.
For most concussed individuals, symptomatic recovery occurs within 2-10 days of the injury. However, concussion can progress to a “post-concussion syndrome” (PCS) which can persist for a few to several months:
As defined by the International Classification of Diseases (ICD 10) criteria, PCS can be diagnosed when there is the development of symptoms in at least 3 of the following 6 categories within 4 weeks of the concussion:
- Headache, dizziness, fatigue, noise intolerance
- Irritability, depression, anxiety, emotional liability
- Subjective concentration, memory or intellectual difficulties
- Insomnia
- Reduced tolerance to alcohol or stress
- Hypochondriacal concerns & adoption of a “sick” role
There are no specific medical therapies for concussion, the mainstay of treatment is true physical and cognitive rest until the symptoms completely resolve (2-10 days), plus the following:
- Good hydration, temporary mild analgesics for headache, anti-nausea medications as needed (but avoid narcotics)
- Education of players, parents and coaches regarding concussion, its associated risks, and principles of safe return-to-play (RTP)
With regard to return-to-play (RTP) following a sports concussion injury, the basic principles are (subject to any more recent clarifications from various organisations/authorities):
- Follow a 6-stage (minimum 6-day) RTP protocol recommended by an international sports concussion consensus group
- The 6-stage protocol ONLY applies in the days AFTER complete resolution of all concussion symptoms
- Each stage is 24 hours, transitioning from no activity, to light aerobic exercise, sport-specific drills without head impact, then more complex non-contact training drills, then full contact practice, and then actual return to the field; if any symptoms develop during any of the 6 stages, the player should rest until the symptoms resolve, and then recommence the 6-stage protocol
- BUT, IF SYMPTOMS PERSIST, OR IF CONCERNING SYMPTOMS DEVELOP, THE PLAYER NEEDS TO BE BROUGHT TO MEDICAL ATTENTION IMMEDIATELY
- RTP should be no less than 7 days AFTER complete symptom resolution for adults and no less than 14 days AFTER complete symptom resoluion for those < 18 years old
- The above RTP guidelines may be more applicable to a first, mild / self-limiting concussion in a given season
- There should be a prolonged absence from play if the player has sustained 2 or more concussions in a season or if the severity of his/her symptoms are greater than the expected severity of the impact itself
For further details on concussion and its management, including return-to-play guidelines, and for information about “chronic traumatic encephalopathy” (CTE; which is an emerging medical and medicolegal concern in multiply-concussed players), see:
- The SPORTS CONCUSSION REVIEW ARTICLE by Dr Khurana, by clicking here (PDF)