Awake Craniotomy
Welcome to Dr Khurana’s Awake Craniotomy pages.
Images shown here are with the permission of Dr Khurana’s patients, for educational purposes.
- Dr Khurana: Awake Brain Surgery Team in Action (Video, 3.5 minutes, 2018)
Panel above: This lady presented with a very large and aggressive primary brain cancer, a GBM. Her brain was swollen, and without surgery she would have lived a few weeks at most. I operated on her twice over a period of eight years, both surgeries were undertaken while she was awake, comfortable and interactive with us. Her survival from a GBM (eight years) was far more than the average survival for this tumour (1.5-2 years). Note the incision, which was photographed one week after her first surgery (green arrows). I use minimally invasive microsurgical techniques for my awakes.
This page has information about the following:
- What is an awake craniotomy?
- Why is an awake craniotomy carried out? i.e., What is its main advantage?
- Is an awake craniotomy the right choice for me?
- Are there any disadvantages of awake craniotomy?
- Will I be in any pain during awake brain surgery? What can I expect?
Please see our Multimedia page for information about the following:
- What is Dr Khurana’s experience with awake craniotomy patients?
- [Includes MULTIMEDIA – Publicly available press reports on some of Dr Khurana’s awake surgeries]
What is an awake craniotomy?
Awake craniotomy is a neurosurgical art that uniquely combines training, advanced technology and microsurgical techniques and, perhaps most important of all, meticulous teamwork, preparation and communication. During some designated part of the operation, the patient is gently awoken by the team in order to be interactive with, and neurologically testable by, members of the team during the surgery. Via the techniques I use, typically:
- Only a small amount of scalp hair is shaved;
- The incision and craniotomy are of a ‘minimal’ footprint as safely possible;
- The patient can NOT hear or feel the ‘drilling’ part of the craniotomy (we have surveyed numerous consecutive awake craniotomy patients of mine to verify this; British Journal of Neurosurgery 2011).
Its key advantages are:
- Enhanced safety via awake testing during the procedure [THIS CAN LOWER PERMANENT COMPLICATION RATES];
- Facilitating removal of more tumour volume especially for lesions in “high-price real estate” of the brain [THIS CAN ENHANCE SURVIVAL];
- Avoidance of prolonged inhalational anaesthesia (use of short-acting intravenous anaesthetics instead)
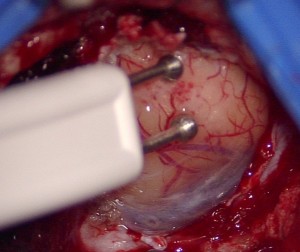
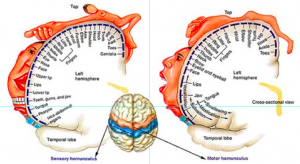
The part for which a patient is awoken is usually the “critical part” of the surgery, for example, involving removal of a brain tumour (e.g., glioma, or a brain cancer such as glioblastoma or metastasis) or cavernous malformation / cavernoma, where the tumour is located in a highly important brain location (i.e., “eloquent brain” aka “high-price brain real-estate”). The surgeon’s tumour resection is guided by a combination of electrophysiological testing (brain micro-electrical stimulation – see image below) and the real-time bed-side testing results from the patient (e.g., the patient’s language, vision, movement and/or touch-sensation) as tested during the surgery.
The key goals of awake craniotomy are to try to maximise the quantity of a patient’s life and minimise the risk of compromising their quality of life. The overall safety and efficacy of this procedure have been demonstrated in an evidence-based manner through cumulative experience with thousands of neurosurgery patients worldwide over decades.
Why is an awake craniotomy carried out? i.e., What is its main advantage?
Awake craniotomy is carried out or recommended to be carried out in SOME neurosurgical patients. Its purpose (i.e., the purpose of the patient being awake during the critical part of the operation) is to make the operation safer (i.e., reduce the likelihood of a neurological impairment or “deficit” in that particular patient). CERTAIN or “SELECT” PATIENTS with brain tumours or vascular malformations involving highly eloquent(i.e., highly functionally important) parts of the brain may benefit from an awake craniotomy because the neurosurgeon can be assured of the neurological progress of the patient in real-time.
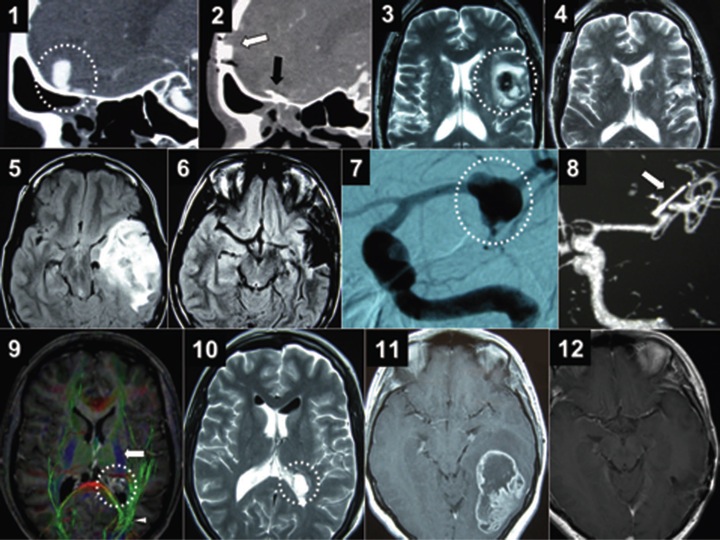
The collage below (from an original study by Dr Khurana and colleagues, published in the British Journal of Neurosurgery in 2011) shows corresponding pre- and post-operative images from a series of awake craniotomies carried out by Dr Khurana for a variety of complex brain conditions including:
- A large venous aneurysm near arteries supplying the patient’s eyes (panel 1 below is a pre-operative CTA image; panel 2 is the corresponding post-operative CTA image following clipping of the aneurysm through a keyhole approach while the awake patient’s vision was being tested by the team in real-time).
- Brain language centre cavernous malformation/cavernoma (panel 3 below is a pre-operative MRI image; panel 4 is the corresponding post-operative MRI image following microsurgical removal of the cavernoma while the awake patient’s language and movement functions were being assessed by the team in real-time).
- A large infiltrating low-grade glioma / primary brain tumour (panel 5 below is a pre-operative MRI image; panel 6 is the corresponding post-operative MRI image following an excellent and safe debulking of the tumour while the awake patient’s language and movement functions were being tested by the team in real-time).
- A large fusiform arterial aneurysm causing language dysfunction in the patient (panel 7 below is the pre-operative angiogram; panel 8 is the post-operative CTA following successful clip reconstruction of the aneurysm while the awake patient’s language and movement functions were being tested).
- A deep symptomatic cavernous malformation in the brain near the vision (optic) pathways (panel 9 is a pre-operative MRI image of the cavernoma with colour tractography overlay; panel 10 is the corresponding post-operative image after complete microsurgical excision of the cavernoma in the awake patient who was being neurologically tested during the surgery).
- A large infiltrating brain cancer (glioblastoma multiforme, WHO grade 4 of 4 primary astrocytic brain tumour) in the patient’s language area, and near her vision pathways (panel 11 below is a pre-operative contrast MRI image of the cancer; panel 12 is the post-operative MRI image after complete macroscopic removal of the tumour during awake neurological testing by us). This patient has outlived the statistics for primary brain cancer, alive at almost 8 years after this awake craniotomy.
It is now well established that the MORE VOLUME a surgeon resects/removes of a brain cancer (glioblastoma multiforme, anaplastic astrocytoma, or a metastasis) or a “low grade” brain glioma (e.g., WHO grade II astrocytoma or oligodendroglioma), the better the prognosis is for that patient. However, the surgical goal must be for “maximal safe resection” – i.e., the surgeon should remove the most he or she can without permanently harming the patient.
In the setting of an awake craniotomy, a neurosurgeon can potentially be more aggressive with the condition (such as a brain cancer) knowing that the patient is awake and responsive and stays neurologically intact as the tumour removal or resection proceeds while the patient is simultaneously functionally tested by other members of the team.
Therefore, the key advantage of awake craniotomy over its traditional anaesthetised/fully asleep counterpart is that it can facilitate a surgeon reducing the risk of permanent neurological complications while increasing the extent/volume of the mass’ resection, through real-time neurological feedback (via micro-electrical stimulation of the brain and awake patient clinical testing) as the surgery proceeds.
Thus, many lesions that would otherwise be deemed ‘higher risk’ of permanent deficit or only partially resectable or “for biopsy only” owing to their location, may be more amenable to safer and more complete surgical resection using this approach.
Is an awake craniotomy the right choice for me?
Awake craniotomy/awake brain surgery may be very appropriate for you if:
- You can tolerate the concept of undergoing some part of the neurosurgical procedure in a fully awake state; and
- You have a condition such as a brain tumour or vascular malformation that is located in or very close to a highly functionally important oreloquent part of your brain; and
- Your neurosurgical team is experienced and comfortable with such an approach, and the neurosurgeon and anaesthetist take the time and effort to explain the expected procedure to you in appropriate detail prior to the day of the operation.
Are there any disadvantages of awake craniotomy?
There are no significant downsides to this approach if all of the three criteria mentioned above are met. Any chance of a seizure, airway difficulty or pain/discomfort are reduced by the appropriate measures undertaken by a well-trained team.
Will I be in any pain during awake brain surgery? What can I expect?
In the hands of an experienced neurosurgical team, you will not be in any pain during awake brain surgery. Why? Because:
-
- Appropriate local anaesthetic nerve blocks are administered around the scalp while you are asleep and prior to the commencement of surgery and before any incision is made, to allow those tissues to go numb for the duration of the procedure. Such nerve blocks can last up to 8 or so hours, while awake craniotomies are typically completed in less than 4 hours by Dr Khurana from the time of the nerve block to skin closure.
- The anaesthetist adminsters certain medications in precise amounts to allow you to be asleep during some of the noncritical parts of the procedure, and awake for the critical parts, or as desired.
- The brain itself feels no pain.
In the peer-reviewed and published experience of Dr Khurana’s awake craniotomy patients (see the next page), the vast majority of patients: experienced little or no pain/discomfort; were satisfied with their experience; and had no intraoperative problem or permanent complication from the surgery.
Approximately one-third of the patients had no recall of the surgery, while one-third had partial recall, and one-third had considerable recall, e.g., team members, conversation and testing — but not the craniotomy itself (as they were intentionally kept asleep for that part of the surgery).
Find out more at: Awake Craniotomy MULTIMEDIA