MVD for Trigeminal Neuralgia, aka ‘Tic’ Facial Pain
Welcome to Dr Khurana’s MVD – Microvascular Decompression / Trigeminal Neuralgia page.
Images shown here are with the permission of Dr Khurana’s patients, for educational purposes.
- Dr Khurana’s MVD Video can be accessed via the link at the bottom of this page.
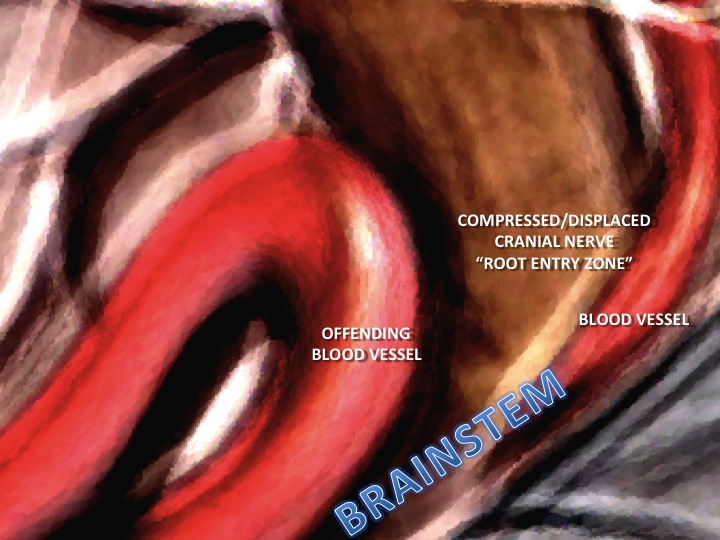
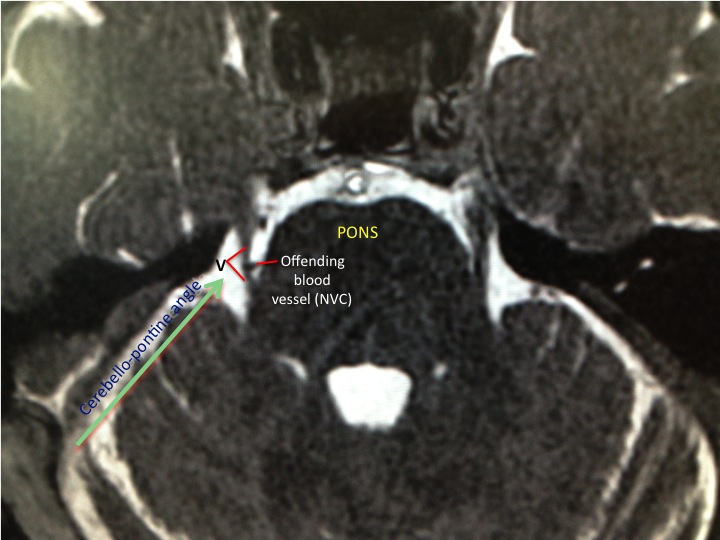
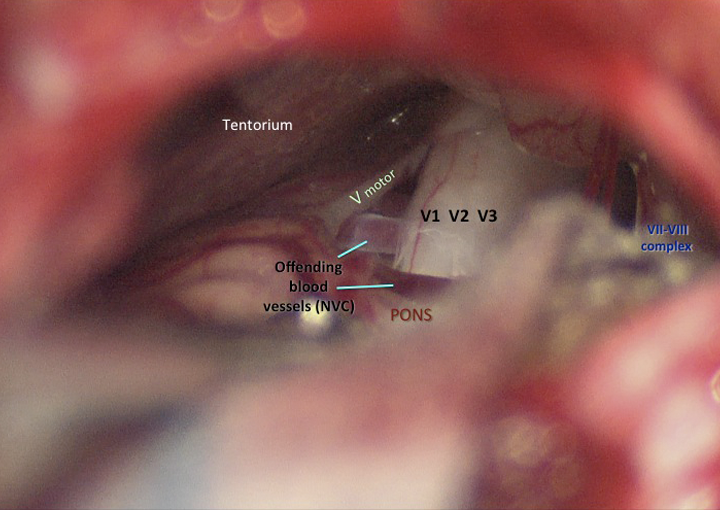
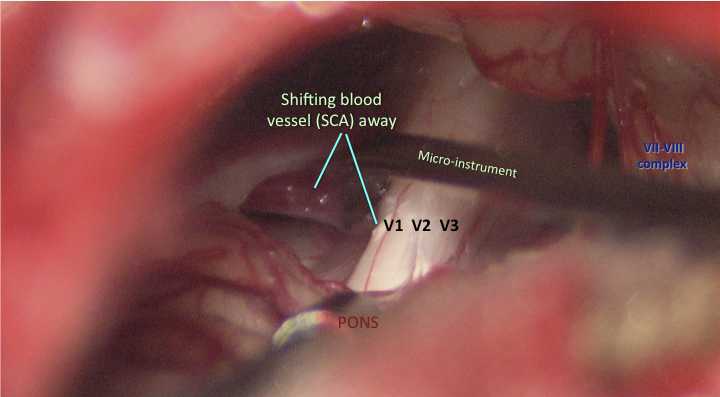
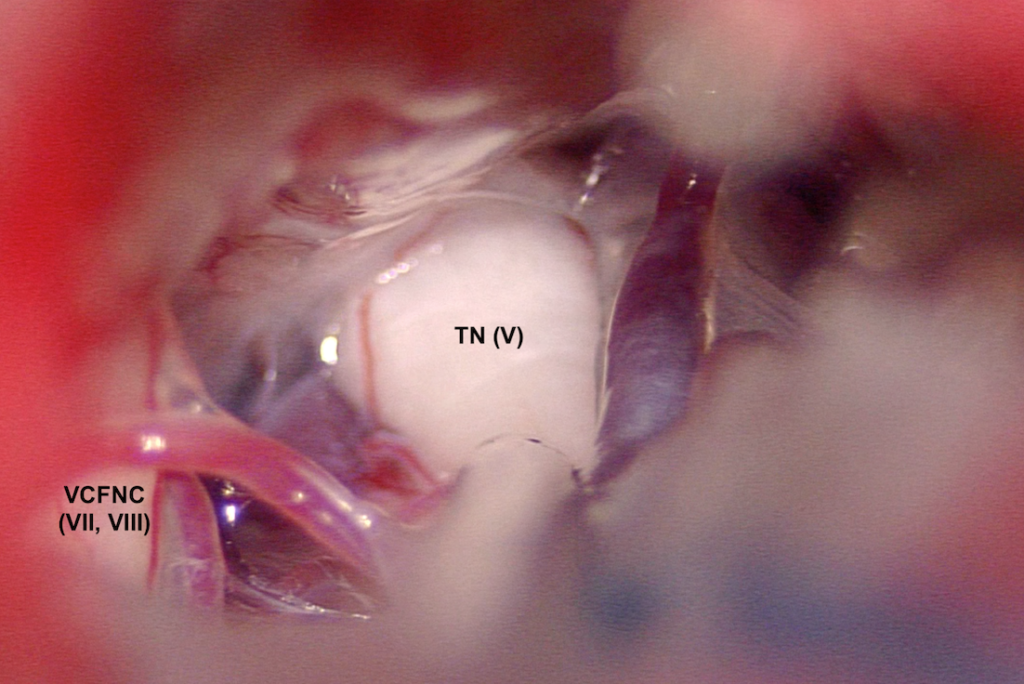
Typical trigeminal neuralgia (facial tic) patients suffer from terrible electrical “lancinating” pain in the face. The pain arises from a physical conflict between a brainstem artery (usually one or more branches of the “superior cerebellar artery“) and the trigeminal nerve (Image 1) at its brainstem (pons region) entry region (“root entry zone“). This physical “pulsatile” neurovascular conflict (NVC; Image 2 FIESTA or CISS MRI image) causes abnormal (“ephaptic“) transmission in the nerve, and this manifests as the severe bouts of pain that is often triggered by, e.g., teeth-brushing, wind on the face, stroking the face, chewing, talking etc. The pain is often incredibly debilitating, sometimes it lessens and then returns with severity.
If the pain does not respond well to medications from your G.P. or neurologist, the condition can be readily treated by a suitably experienced cerebral microsurgeon in an operation referred to as microvascular decompression (MVD).
I often encounter patients who have suffered for years with debilitating trigeminal neuralgic/tic facial pain before having the MVD/microvascular decompression surgery under my care. I have written a blog on this (Please click here to access that blog, and then use the link at the bottom of that blog to return to this page).
Patients with trigeminal neuralgia should NOT feel that “nothing can be done” for their pain, NOR should they undergo any potentially destructive radiation of the brainstem as the first-line treatment, when there is a typically safe and effective time-tested and minimally invasive microsurgical solution that does not involve any entry into or destruction of brain tissue.
Patients with suspected trigeminal neuralgia should be appropriately imaged (via, e.g., dental OPG and brain MRI/A) to ensure that there is no tooth abscess, or any multiple sclerosis plaque or other structural lesion (i.e., skull base or posterior fossa tumour or vascular mass) in or near the ‘pons’ and/or trigeminal ganglion and/or skull base trigeminal nerve branches, that may be causing the facial pain.
- Image 1
- Image 2
Click images for larger view
Sometimes the actual site of neurovascular conflict is not identified by the reporting radiologist. Here’s an example: This patient whose scan collage is shown below had severe longstanding right V3 and V2 trigeminal neuralgia. On this zoomed up fine-cut posterior fossa MRI (CISS/FIESTA sequence), I can see a branch of the right superior cerebellar artery (SCA) impinging upon the root entry zone (REZ) of the right trigeminal nerve as the nerve emerges from the lateral pons. The radiologist, however, reported the study to show no cause for the patient’s symptoms. I have highlighted where the conflict is occurring (between the different colour arrrow tips).
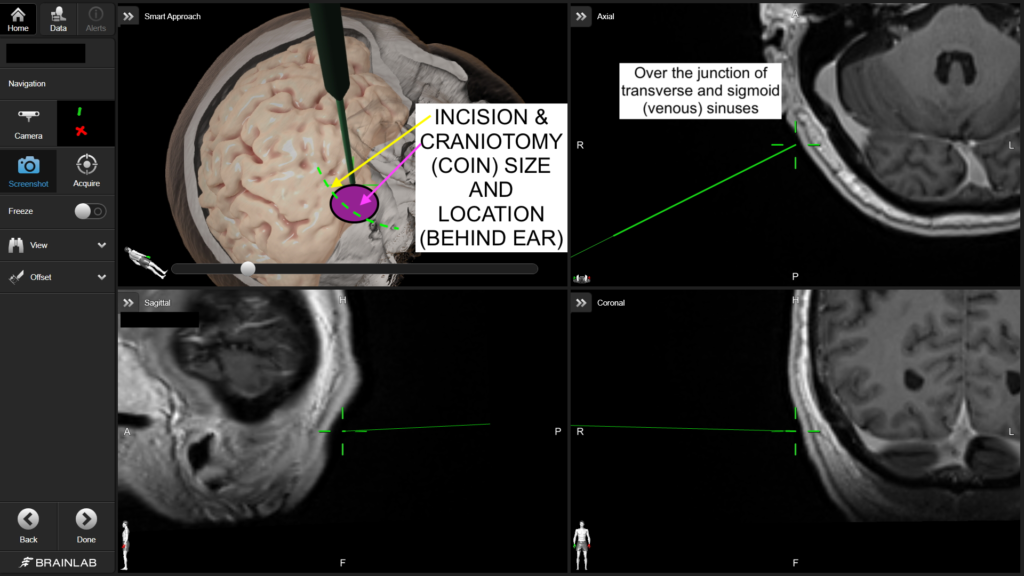
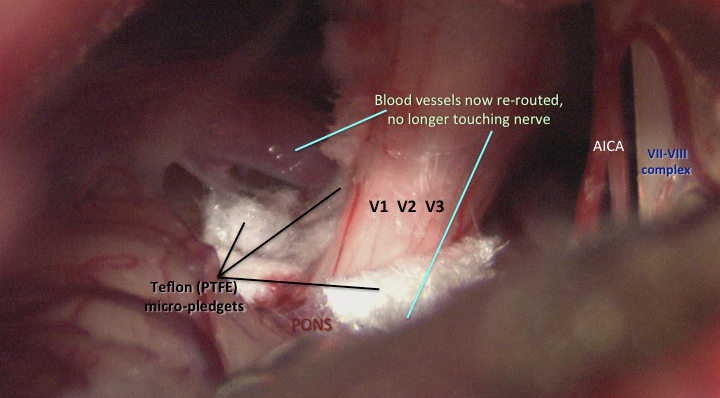
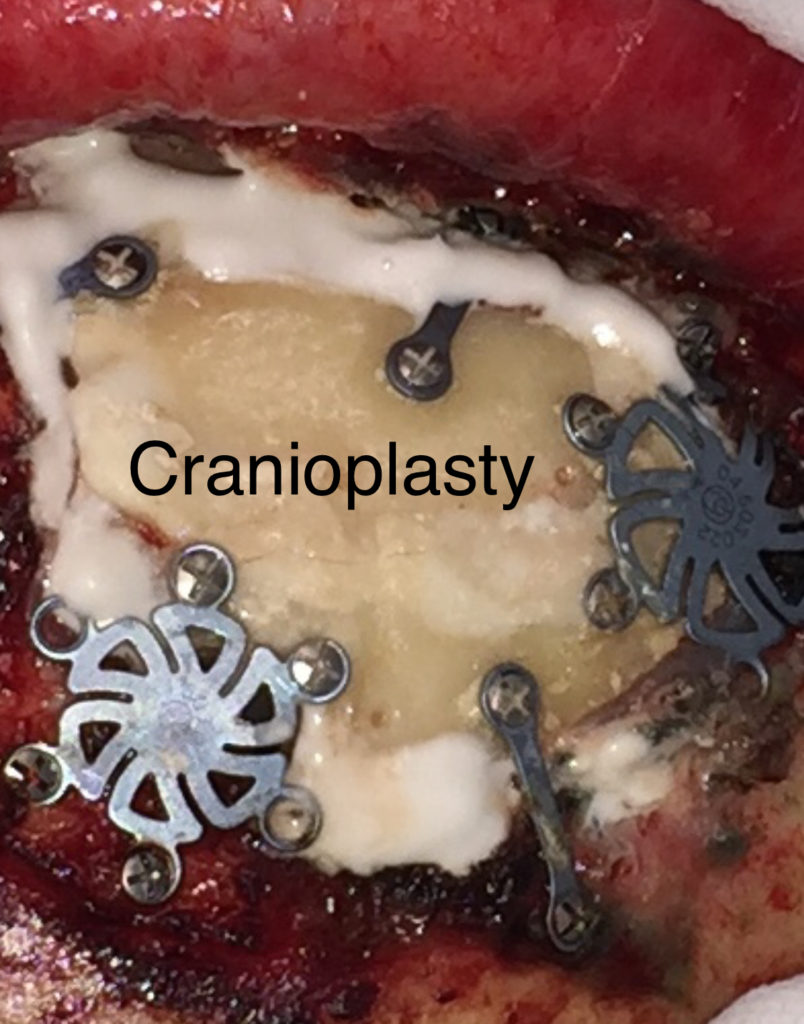
I have nearly 20 years of neurosurgical experience with MVD microsurgery, with overall excellent and enduring results for my patients to date. Meticulous microsurgical technique (click the video link at the bottom of this page, for an example from one of many such surgeries), careful patient preparation and positioning, and a focus on patient safety are key to this (e.g., real-time nerve monitoring, nerve stimulation, temporary lumbar CSF drainage, neuronavigation, and meticulous attention to detail). I use a small ‘boomerang-shaped’ incision behind the ear, a small/mini-craniotomy (less than the size of an Australian 20 cent coin), and advanced retractorless microsurgical techniques to access and decompress the trigeminal nerve complex.
- Image 3
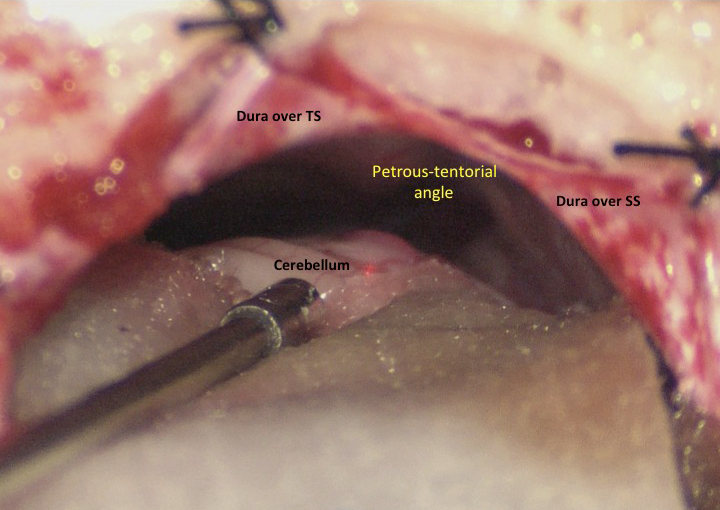
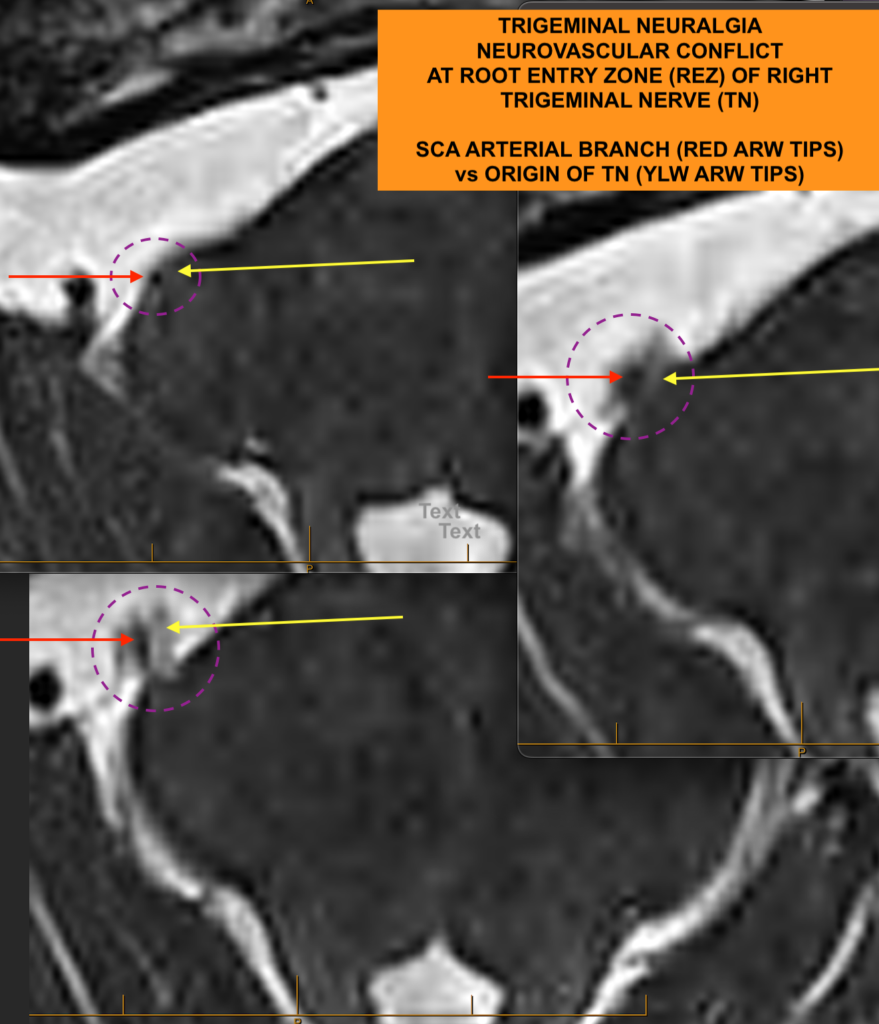
- Image 4
Click images for larger view
The trigeminal nerve is surgically decompressed using a combination of micro-instruments to free up the local neurovascular tissues, followed by placement of tiny (1-1.5mm) pledgets of teflon (PTFE) between the offending vessel(s) and the trigeminal nerve trunk. I use a total of 4 technical steps to improve the anatomy and physiology of this brainstem region, for the better. My craniotomy reconstruction techniques are carefully designed to provide structural and cosmetic integrity.
- Image 5
- Image 6
- Click this link to watch Dr Khurana’s MVD / Microsurgery Video (with thanks to Twin Turbo Productions)