Trigeminal Neuralgia: Patient 78 years, medically refractory facial pain, wants no pain and no more Tegretol. Understood. Travelled to us. Done.
This lovely gentleman of 78 years, is the most senior Trigeminal Neuralgia (aka ‘Tic‘ facial pain) patient that I have operated in my years of doing this beautiful (at least, to a neurosurgeon) microsurgical procedure. Age 78. I think it’s a sign of the times, with people living longer and understandably wanting fulsome and happy, healthy lives. He cycles 200km/wk, a retired businessman, and told me he had done ‘a tonne of research’ into his condition and his options before deciding to travel to Sydney from interstate for his microvascular decompression (MVD) under my care, and that of the excellent team I work with. For his stated age, he looked to be in very good health and constitutionally robust when I teleconsulted with him and discussed his referral and medical work-up to date.
The patient was discharged a week after his surgery, TN pain-free from the time he woke up post-op. I hold on to my TN/MVD patients for a little longer (i.e., until one week post-op.) to ensure they are independent and confident prior to their discharge. The extra few days pays dividends in their recovery.
Patient safety and a good outcome are all that matter here. So, to try to ensure that every time, I and the wonderful people I work with during such operations and post-op., ensure:
- Insertion of a lumbar drain prior to incision (to relax the cerebellum so no self-retaining retraction is required upon it during access);
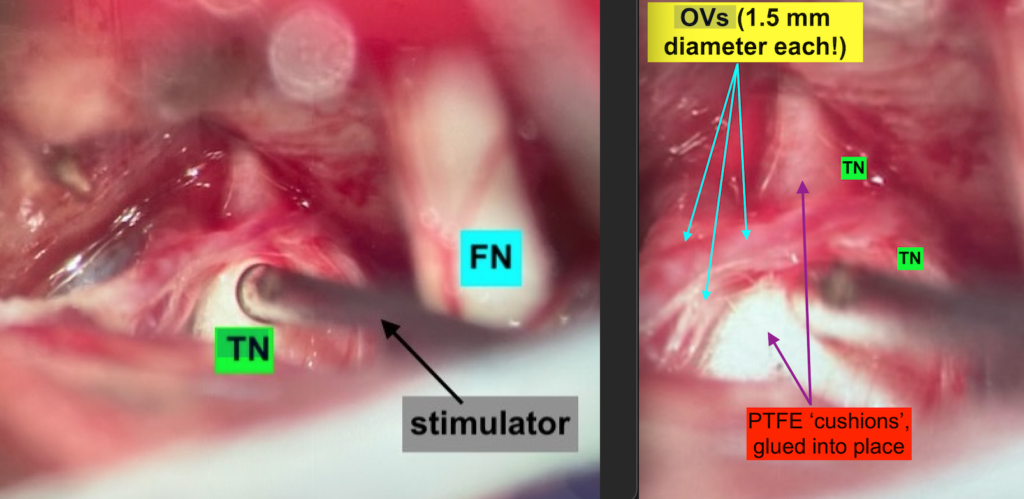
- Neuromonitoring in real-time from the get-go (cranial nerves V, VII, VIII/BAER, MEP, SEEP) and microstimulation (to check V vs. VII whenever needed);
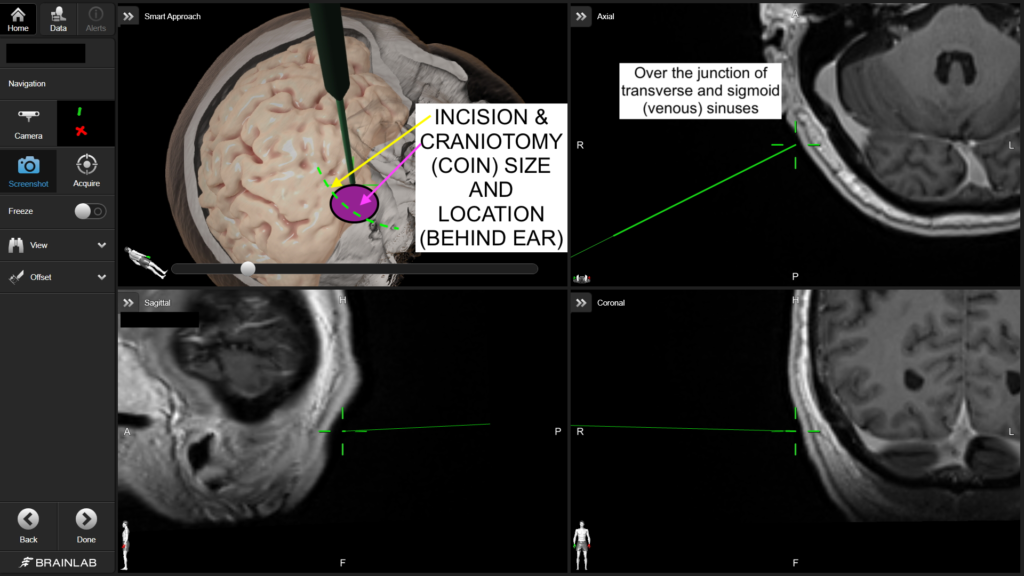
- Neuronavigation (I use my Brainlab system for this; this ‘brain GPS’ is a good adjunct to anatomical landmarks in planning);
- Microsurgical technique and instrument optimisation (thank you doctors Fred Meyer, Dave Piegras and Robert Spetzler, the three US grandmasters I trained under during my decade in the US, and Kogent Surgical for my personalised micro-instrument tray);
- Ideal bio-prosthetics for cranial reconstruction;
- Post-op. ICU (minimum one night) and CT (e.g., to exclude the presence of any untoward blood and air);
- Daily bedside in-patient physiotherapy (for gait and ADL clearance before discharge);
For more information on trigeminal neuralgia and microvascular decompression (including a video link at the bottom of that page), please visit our main TN page.
< Back to blog